“Is Everyone Looking At My Skin?” How I Was Blindsided By Adult Eczema
:max_bytes(150000):strip_icc()/VWM-derm-2-everyone-looking-at-my-skin-b-1b0db83438b743279c48639bbc7d4170.jpg)
Eczema is so common that it has worked its way into a Megan Thee Stallion lyric, yet when it snuck up on me, I didn’t recognize it. It was the peak of a particularly humid New Jersey summer, and I assumed the irritation on the side of my foot was from the friction of it rubbing against my jewel-encrusted pool slides.
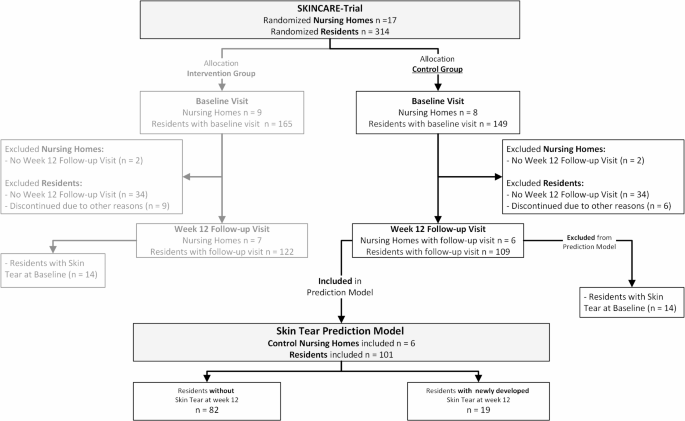
But when the irritation went from barely noticeable to consistently annoying, I sought out medical advice. Also known as atopic dermatitis, eczema is a chronic skin condition that causes itching and dryness. It deeply impacts our self-perception and the way that we are perceived by others.
Self-Perception and Atopic Dermatitis
This was something that I had watched several kids face in classrooms while growing up, but I had no idea it could sneak up on you later in life. I was completely blindsided by its appearance.
“It’s actually way more common than you would expect,” says dermatologist Dr. Hannah Kopelman. “I recently saw a patient in his 90s who had his very first flare of eczema. People think it just happens in young babies or kids.”
The discomfort was bad, but the visible symptoms were worse. I hated the way my skin was raised, interrupting the natural lines of my fingers and toes. I wondered, was everyone looking at my skin?
Body Image Concerns
The presence of the symptoms felt like a shadow looming over my summer. Concerns about being seen as ashy swirled in my head. I felt embarrassed. The last thing I wanted was for people to think I had some sort of contagious rash.
I recently saw a patient in his 90s who had his very first flare of eczema. People think it just happens in young babies or kids.
My sense of embarrassment was validated. According to The Journal of Allergy and Clinical Immunology: In Practice, “social embarrassment” can be caused by eczema, and “Individuals with atopic eczema may be more likely to experience depression and anxiety through the effects of itch and discomfort, disfigurement, and perceived social-stigmatization.”
Embarrassment and shame surrounding eczema persist despite how frequently it appears in so many lives.
“We always tell patients this is such a common disease, and so many people struggle with it,” says dermatologist Dr. Hannah Kopelman. Coping might be easier when you do it alongside others. Dr. Kopelman points out spaces where those with eczema can come together to discuss their challenges.
“You’re not alone. There are support groups that you can connect with where other people can really relate to what you’re going through,” she says. She adds that there is always something a person can pick apart about their appearance. “Everyone has something. So it might not be this, but they have something else.”
Self-Consciousness and Social Interactions
A 2018 article in the BMJ Open Journal reports that “Patients with chronic skin disease can display a fear of negative evaluation and perceived stigmatization. Patients with visible skin lesions are reported to be more likely to have fear of social rejection together with fear of negative evaluation by others either within their peer group or from others.”
This can lead to self-isolation. Someone with eczema might decline an invitation when they are experiencing a flare-up for fear of being faced with awkward questions about visible or exhibiting signs of discomfort. Even if your eczema is mild, that unbearable prickly feeling it comes with does not help you serve the friendly cocktail party energy you’d like to.
Not to mention, the fear of stigmatization is ever-present.
According to The National Eczema Association, half of patients with moderate to severe atopic dermatitis admit that it significantly limits their lifestyle, and up to one-half of adults with atopic dermatitis avoid social interactions due to their appearance. Case in point: I would not attend something that required me to wear sandals if my eczema was bothering me—and being forced to chat about it was not something I was interested in.
I was uncomfortable discussing my eczema until I couldn’t put it off anymore. I was even nervous to bring it up with my doctor. However, it’s important to be open with your healthcare provider so they can help you work on managing the condition.
Ironically, talking can help one cope with the type of social anxiety that eczema can cause. Seeking professional help, breathing techniques, reframing, and venting in a safe space are also helpful coping mechanisms.
Psychological Effects
The psychological effects of eczema are significant. For example:
Sleep disturbances: According to the Journal of Investigative Dermatology, “Having eczema and concurrent sleep disturbance also significantly increases the risk of psychological disorders.”
Emotional turmoil: A 2020 article in the Journal of the European Academy of Dermatology and Venereology reports that “anger, frustration and psychosomatic states have been found to affect atopic eczema symptoms.” Psychological issues can also exacerbate eczema.
Role of Healthcare Providers
Some people become so upset by their eczema that they opt out of participating in social activities and skip out on professional commitments. “I have seen people lose their job or not be able to go to school because of skin problems, and it’s important for me to make a patient feel confident that that’s not going to happen to them,” says Anna Chacon, MD, FAAD.
Taking a holistic approach helps Chacon and other like-minded healthcare professionals address the whole patient and not just what is on the surface of their skin. This is critical because, eczema in late adolescence is associated with suicidal ideation and mental health problems, while adults with atopic eczema are more likely to develop new depression and anxiety.
To address what is on the surface, there are multiple over-the-counter and prescription options to help manage eczema, such as oral medications, injections, and topical creams that can completely clear the skin in certain cases. Certain people have success with changing their diets and environments. Being honest with your healthcare provider can help you get the best combination of therapies for your specific eczema.
“[If] you’re not improving or you’re kind of hitting a plateau, then we have other options, and we can always change to other medications,” Chacon adds.
“Reducing your exposure to potential irritants can go a long way in terms of managing your eczema and future flareups,” explains dermatologist Dr. Melanie Palm, MD, MBA. “Eczema triggers can vary from person to person, so it is important to understand what your specific triggers are.”
Links and Resources
If you’re dealing with eczema/AD, there are regional and international support groups you can turn to for assistance. For more information about eczema, visit the National Eczema Association.
link

:max_bytes(150000):strip_icc()/KeyairaBooneheadshot-3eb1e00526a742e1bc368f8841d1e45f.jpg)