Kalydeco slows CF disease progression over time, study finds
Treatment with Kalydeco (ivacaftor) for almost eight years consistently improved lung function and reduced mortality in people with cystic fibrosis (CF), according to a study looking at several measures of disease progression.
The therapy also significantly improved nutritional status, which together with reduced pulmonary exacerbations, hospitalizations, and lung transplants lowered the burden of healthcare costs. “These findings reinforce the existing real-world evidence that [Kalydeco] can slow disease progression and decrease the healthcare burden of CF over the long term,” the researchers wrote.
The study, “Long-term impact of ivacaftor on mortality rate and health outcomes in people with cystic fibrosis,” was published in Thorax.
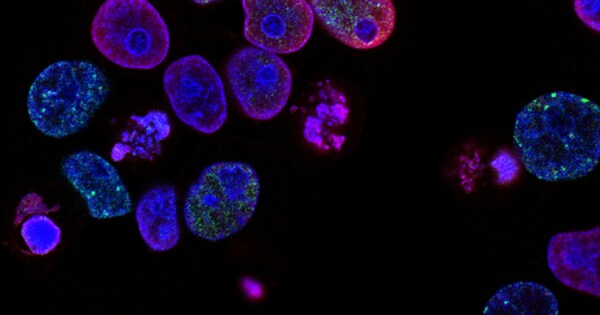
CF is caused by mutations in the CFTR gene, leading to no or faulty production of the CFTR protein. This results in the accumulation of thick and sticky mucus, particularly in the lungs and in organs of the digestive system.
Kalydeco was the first CFTR modulator to be approved. A CFTR modulator is a type of therapy designed to treat CF caused by gating mutations (in which the gate-like CFTR protein cannot open normally). It works by increasing the time the gate is open, enhancing CFTR activity. The number of eligible mutations has been expanded multiple times since the original U.S. approval in 2012.

Data taken from patient registry
Real-world studies for up to five years demonstrated the treatment preserved lung function and improved patients’ nutritional status, while reducing pulmonary exacerbations (a sudden drop in lung function, usually due to infection), hospitalizations, and risk of death.
This study analyzed the long-term impact of treatment with Kalydeco on people with CF in the U.S., using data from the U.S. Cystic Fibrosis Foundation Patient Registry. Participants were started on Kalydeco between January 2012 and December 2018, and all had at least one year of follow-up.
A total 736 CF patients with at least one gating mutation (except R117H and mutations that render CFTR’s function minimal) were treated with Kalydeco during the study period. These patients were matched by age with a control group of 733 patients with one copy of the F508del mutation — the most common CF-causing mutation that affects protein processing — and a minimal CFTR function mutation, who had not been treated with CFTR modulators.
Patients in both groups were 6 and older, and had clinical data available for at least 24 months at the time of study enrollment. Almost half were women, and more than 90% were white.
Over a maximum follow-up period of almost eight years, patients treated with Kalydeco had a 78% lower mortality rate than the control group. Mortality risk was also lower in Kalydeco-treated patients when looking at consecutive one-year periods.
Disease progression measures improved
Kalydeco also significantly improved lung function relative to the controls, as reflected in a measure called percent predicted forced expiratory volume in 1 second, an assessment of how much air a person exhales after a deep breath. The mean difference increased with time, from 7.98 after one year to 10.95 after five years, and was more significant in patients aged 12 to 17.
“These data suggest that [Kalydeco] leads to better lung function that is sustained with long-term use,” while “highlighting the importance of treatment during adolescence, a period characterized by rapid lung function decline,” the researchers wrote.
Long-term treatment also reduced the rate of lung transplant by 89%, and the rate of pulmonary exacerbations by 51%.
“The sustained reductions in [pulmonary exacerbations] with long-term … treatment may contribute to the reductions in mortality and lung transplant and the improvements in lung function,” the researchers wrote.
In patients 20 and older, those treated with Kalydeco had a significantly higher mean body mass index (BMI), a measure of body fat based on height and weight, indicating better nutritional status.
And BMI z-scores — which compare an individual’s BMI to a standard growth chart — were significantly higher in patients aged 6 to 19 treated with Kalydeco, compared with controls. Long-term treatment also reduced all-cause hospitalizations by 50% and outpatient clinic visits by 15%.
“Our analysis suggests that [Kalydeco] provides sustained clinical benefits in people with CF over a follow-up period of approximately 8 years,” the researchers wrote.
link